
Thanks to Dr Julie Barrett, Research Coordinator for the Housing and Dementia Research Consortium (HDRC) for this week’s blog.
What does “build back better” mean for people living with dementia in extra care and retirement housing in the UK?

In its second webinar of 2021 the HDRC and guest presenters explored how extra care and retirement housing needs to change and prepare for the future with respect to residents living with dementia, bearing in mind Covid-19 is not going away and will not be the last pandemic we experience.
The 2021 All-Party Parliamentary Group (APPG) report ‘Housing for people with dementia – are we ready?’ states:
“The restrictions imposed in response to Covid-19 have highlighted existing challenges to housing providers. Many people affected by dementia have reported deterioration of their condition, but also an increased reticence to move to a care or nursing home. Creative solutions have been adopted by housing providers, often as a result of the property services, housing management and care teams working together. These examples of best practice need to be shared across the sectors.”
According to the World Economic Forum, Covid-19 is not an aberration. It is in fact part of a pattern of increasingly frequent epidemics, thus it is vital that we share good practice now, during the current epidemic, in order to reduce future risk.
The webinar was chaired by Jeremy Porteus, Chief Executive of the Housing Learning and Improvement Network and there were 4 topics of discussion:
- APPG report, ‘Housing for people with dementia – are we ready?’ How do we use the findings and recommendations to move forward? – Wendy Wells and Jeremy Porteus, Dementia and Housing Working Group
- Design and development of dementia-friendly housing to minimise the spread of infection –John Walker, Walker Simpson Architects
- Management of dementia-friendly housing post Covid-19 – Kris Peach, Housing 21
- Loneliness among residents living with dementia during the pandemic and rebuilding relationships and communities – Michael Roberts, ExtraCare Charitable Trust
To end the webinar there was a session where housing providers of the HDRC Steering Group spoke about supporting staff post lockdown.
APPG report, ‘Housing for people with dementia – are we ready?’ How do we use the findings and recommendations to move forward?
To kick off the webinar, Jeremy Porteus spoke about the inquiry of the APPG on Housing and Care for Older People and the resulting report ‘Housing for people with dementia – are we ready?’

The APPG inquiry was chaired by Lord Best, comprised four sessions over eight months, and brought together people living with dementia and carers, parliamentarians and experts from the field, and verbal and written evidence. There were five areas of focus, corresponding to the five chapters in the report:
- What older people told us about their housing experiences and living with dementia
- Understanding dementia and planning for the best possible housing options to be available
- The importance of housing choice within communities
- Using technology and making adaptations to improve the wellbeing of people affected by dementia
- Every decision about care is also a decision about housing
The inquiry identified 20 key issues with the report making just over 40 recommendations aimed at different groups, and Jeremy picked out a few relevant to the webinar:

The APPG report can be found on the Housing LIN Website
Following on from Jeremy was Wendy Wells, Head of Policy and Business Implementation at Guinness Care, who introduced the Dementia and Housing Working Group (DHWG) and how this group intends to use the findings and recommendations of the APPG report to move forward.
The working group was initially established by the National Housing Federation a number of years ago and is currently chaired by Vanessa Pritchard-Wilkes, Head of Strategic Influence at Housing 21. The group is made up of a number of housing associations, Government departments and other organisations and networks who have an interest in housing and dementia, including the HDRC, and its purpose is to advocate the role of appropriate housing in enabling people to live well with dementia. Together with the Alzheimer’s Society, the Dementia and Housing Working Group produced the Dementia-Friendly Housing Charter, a key deliverable from the Prime Minister’s challenge on dementia.
The DHWG has decided to focus on two specific recommendations, and also the theme of ‘advice and information’ which ran through the report and recommendations.
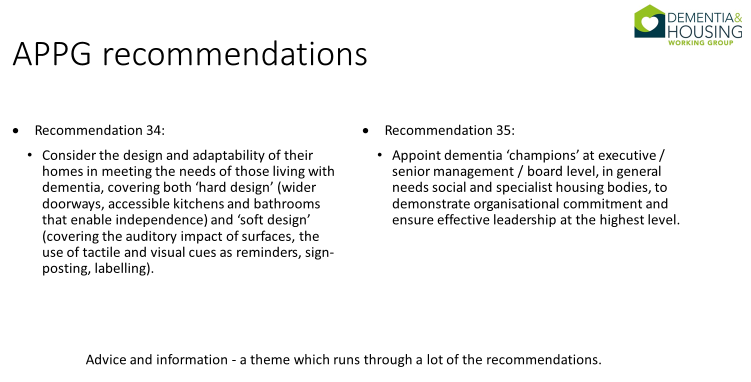
It will do this by establishing task and finish groups to undertake actions against the recommendations. With respect to recommendation 34, all housing providers have design guides, and some have specific dementia-friendly design guides, which most are willing to share. Much the same as ‘housing rising to the dementia challenge’ housing providers will share their knowledge and expertise across the sector to encourage the sector to meet this recommendation. The group argues that good dementia design is good design, for everyone. They will also look to develop case studies to highlight the impact of good design and develop resources which signpost people to the many design resources which are readily available.
With respect to recommendation 35, many housing providers have adopted the Dementia Friends initiative for staff and/or residents. This recommendation seeks to get buy-in at the very top of the organisation to ensure dementia consideration is thoroughly embedded throughout. The group will undertake work to build on this recommendation, suggest what a dementia champion role may look like and the skills and knowledge which it should contain. The group will also develop case studies of organisations which have been successful in their approach to share that knowledge.
In terms of advice and information, the DHWG will develop accessible wording around dementia that people can use on their website to signpost visitors to appropriate resources.
Design and development of dementia-friendly housing to minimise the spread of infection
The next presenter was John Walker, Director of Walker Simpson Architects who spoke about the design and development of dementia friendly housing to reduce the spread of infection. He spoke about the importance of the National Prevention Signpost, bearing in mind Covid-19, colds and flu are all airborne viruses, and about various prevention measures:
- Mitigate Covid-19 transmission in confined spaces;
- Vaccination, Masks, Testing and Supporting those isolating;
- Cleaning regimes and cleanliness;
- Design quality: space and specification, indoors and outdoors;
- Reduce and avoid unnecessary contact, e.g. door handles, physical surfaces;
- Provide Digital Connectivity.
John then described recommendations for design of the physical environment in terms of special, environmental, digital, wellbeing and outdoor improvements, and the use of biophilia in design of the physical environment. He noted that these recommendations closely correspond to the key design principles of the HAPPI (Housing our Aging Population Panel for Innovation) report.
John ended by noting that the World Alzheimer Report 2020 states: “Design for dementia is 30 years behind the physical disabilities movement and this must change” and drew attention to salutogenic design – design for wellbeing – which would include design for disease prevention.
Management of dementia-friendly housing post Covid-19
The third topic of the webinar considered the management of housing over the last couple of years and the lessons learnt, and was presented by Kris Peach, Executive Director of Extra Care at Housing 21. Kris spoke about how underprepared the housing sector was 18 months ago – “few plans survive the first contact with the enemy” – but it is how they learn from this that will stand them in better stead with moving forward. There was a sense of panic with uncertainty about what the best course of action was, different messages coming from different areas, and confusion reigned.
As a national provider, Housing 21 also had a lot of different approaches as to what they should do when Covid-19 broke out, including who they should contact, what actions they should take and where they should follow up. People were being discharged from hospital, sometimes inappropriately, especially in the case of people living with dementia. It was clear that Housing 21 residents and their families and friends were also confused by the situation, and the housing provider had to take some control over that.
Furthermore, there was, and still is, a lack of understanding about the difference between residential care and extra care, and when guidance came out it referred to residential care. There was no real support or guidance for independent living/extra care, so the housing providers themselves had to develop their own guidance. This provided clarity for staff, residents and their families and friends, who were very concerned about how the services were going to continue to be managed in such an environment, particularly for residents living with dementia.

Communication was, and continues to be, the key for managing housing during this time. This meant being clear and decisive, with Housing 21 taking a consistent stance across all services, even when there were some inconsistencies coming from professionals in the industry. Also, remembering that staff were also affected and unsure what they should do personally and for the residents. For residents living with dementia, communication with family and friends was critical, as was working closely with health professional to adapt practices in supporting people living with dementia. There was also the PPE issue to address. Housing 21 had a team of people across the country working to source PPE, and redeployed people to become PPE suppliers – they now have an excess of large gloves, if anyone would like some!
When lockdown came there were difficult decisions to make regarding levels of lockdown and how far they should go. The case was clear in residential care – lock everything down, don’t let anyone in and no family or friends can visit. However, an independent living setting like extra care creates a challenge. Housing 21 adopted the approach that where there were no cases in a scheme the large lounges were left open for residents to use. All visitors were stopped, which created both complaints and support, but protecting residents and staff was a priority.

Social distancing wasn’t always possible, particularly with respect to people living with dementia. The onsite staff and care teams were important in supporting this. Housing 21 is well versed in supporting safe walking with purpose and had developed practices and training for this. For residents who received personal care, Housing 21 ensured that this remained in place. There was also increased cleaning activity on touch points in communal areas.
In terms of learning with respect to residents living with dementia in extra care settings, Kris reiterated John’s message that the physical design of the indoor environment has a big role to play, and the outdoor environment and how it is used is also important. The design of the environment and useable space is important, but it is the people that make a difference. Housing 21 has introduced some different roles and spaces such as dementia advocates, dementia practice leads (who have received specialist in depth training from the Association for Dementia Studies), dementia coaches in every extra care scheme (trained by the dementia practice leads), and dementia practice hubs (a space for staff to come together and share best practice). Technology also has a role to play, such as iPads to enable residents to keep in touch with family and friends. Housing 21 has also been working closely with other residents to provide education about people living with dementia and the language around dementia, and to address stigma and misunderstanding around dementia. One way they have done this is to use the Dementia Friends initiative with staff, contractors, residents, family and friends.
Kris finished by outlining the challenges still faced going forwards, such as design costs, recruiting and retaining staff, and ensuring staff are rewarded for what they do. Finally, Covid-19 is not going away and housing providers have learnt how to operate in a different way in managing their services, some of which will continue to benefit the residents in the long term. Policies and processes are key. They now know how to face the enemy, as compared to 18 months ago, but they must continue to be vigilant and work together to support the most vulnerable people, having a shared interest in achieving the best outcomes and a shared purpose of keeping everyone safe.
Loneliness among residents living with dementia during the pandemic and rebuilding relationships and communities
In the final presentation, Dr Michael Roberts, Engaged Lives Project Officer at ExtraCare Charitable Trust, spoke about how the ExtraCare Charitable Trust is supporting people living with dementia beyond loneliness.
Michael explained that a study by Victor et al (2020) found that just over one-third of people living with dementia in the UK experience moderate or severe loneliness. However, the study also found that people with dementia were no more likely to be lonely than their peers. The factors that are more significantly associated with loneliness amongst those living with dementia are living alone, social isolation, depression, and low quality of life. Interventions should “place more emphasis on helping people with dementia maintain their social relationships and links with their local community.” (Victor, 2020)
So, what can housing providers do to help? Working with loneliness is about dealing with the reality of here and now:
- Ask “what is this individual capable of doing right now to feel more connected?”
- Take steps to anticipate difficulties further down the line
Both should recognise that loneliness is usually a symptom of more fundamental issues.
What is the ExtraCare Charitable Trust doing across its 16 retirement villages and five housing schemes? The Engaged Lives Project addresses the causes rather than the symptoms of loneliness by empowering people to take action on underlying factors:
- Peer-support workshops addressing personal and psychological topics over six weeks
- Visions of older age
- Thinking and behavioural patterns
- Staying mobile
- Dealing with difficult emotions
- Attending to relationships
- Building confidence and capacity to connect in the ways people desire
- Take steps that lessen the likelihood of experiencing loneliness in the present and the future
- Build strong and resilient networks
- Deal with mental health problems before they progress
- Workshops attended by people with cognitive impairment and early-stage dementia
- Empower people to take steps now to anticipate, rather than respond to, loneliness
Michael discussed loneliness being a result of dementia, but also that loneliness is a significant predictor of developing dementia. He made some recommendations based on the literature and what the ExtraCare Charitable Trust has found to work:
- Support people to anticipate loneliness in the future, (both before, and in the early stages of dementia) by addressing underlying factors
- Support people to deal with loneliness in the present by looking out for underlying factors
- Take steps to connect people to help them lessen the likelihood of living with dementia
The ExtraCare Charitable Trust as produced a guide, ‘Steps to Connection’, that is interactive, includes reflective exercises and provides ten steps to support a sense of connection. This can be accessed and used as a standalone resource (individual use) or as a resource for use as part of a structured support package. If you’d like offer this to your service users/residents, please contact: michael.roberts@extracare.org.uk

For more information on dementia and loneliness, the ExtraCare Charitable Trust’s Engaged Lives Project and Steps to Connection resource, click here to see the blog that Michael wrote previously for the Association for Dementia Studies.
Supporting staff post lockdown
To conclude the webinar, housing provider members of the HDRC Steering Group spoke about how they have been and are continuing to support staff through the pandemic. Louise Lee from Platform Housing Group spoke about how it is very much an ongoing journey of learning and adapting, and agreed with much of what Kris said concerning responding, adapting, practical things like cleaning schedules, reassuring staff and clear communication. She stated that much of this continues because they are still on that journey and, post lockdown, there is still some of the sense of the unknown for staff, partly due to the government advice to ease measures now. It is very much about listening to staff teams and residents and thinking about the settings Platform works in. Staff still feel vulnerable in terms of the impact of Covid-19 on their lives. Platform has taken a very steady approach to easing measures post lockdown and has made sure that all properties and services are aligned, e.g. if retirement living staff are wearing masks then staff in the repair services visiting the properties also need to be doing the same. Communication is key. One challenge has been managing the wellbeing of staff who have had to communicate and stay in contact with colleagues virtually. Platform introduced online colleague chats, online executive coffee chats, a wellbeing officer, mindfulness sessions, and mental health and wellbeing sessions. To sum up, it is about talking and listening to staff and taking on board what they are saying. Platform also has an ideas lab where colleagues can put in ideas and suggestions, which is constantly monitored and passed onto senior colleagues to come up with a response.
Michael agreed that it was important to listen to staff and offer support with wellbeing. The ExtraCare Charitable Trust offers mindfulness-based resilience coaching to the senior leadership team which has been well received. They have also found a benefit in bringing staff and residents together for wellbeing sessions, e.g. peace of mind through mindfulness, how to reconnect safely. Having residents and staff share vulnerabilities together has been really useful in terms of the sense of everyone being in this together, building a sense of unity, and residents being more understanding of staff.
Kris stated that the importance of the staff on the frontline was evident from the beginning of the crisis and it is important not to lose sight of that and slip back into the normal ways of working. Housing 21 is working to ensure that doesn’t happen. Reward, recognition and making sure people are paid fairly is really important, and it needs to be there to support the industry properly. Housing 21 is working, with local authorities in particular, to ensure that they pass those fairer rates onto care workers. With respect to talking things over, Housing 21 refers to it as post-traumatic stress and now, a month or two since opening things back up, it feels like everything is back to normal, but there have been some really dark times for staff and residents and it is really important that everyone reflects on that and talks about it so that they can go forward together with a sense of harmony between residents and staff. So, it is a matter of not losing sight of what happened, talking about it, and ensuring the staff on the frontline have got everything they need to do their jobs properly and continue to care for residents.
Guinness care have also put various interventions in place to support staff but the organisation is definitely still feeling the impact of the pandemic. Also, going into winter there is the feeling that people feel worse now than they did this time last year. So, Guinness is working with staff groups to find out what would help them and keep moral high so they can get through what may come this winter.
A recording of the webinar and the presentations are available on the HDRC website.
Connect with the HDRC on twitter @HousingDementia
Connect with ADS on twitter @DementiaStudies and on Facebook @adsuow
